‘The health budget continues to dwindle’

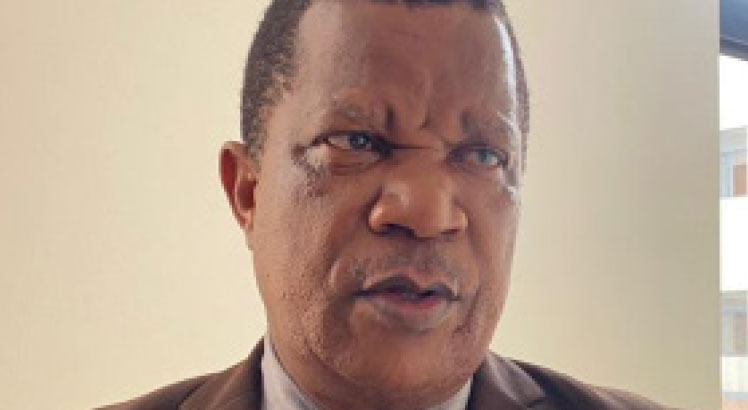
Of late, the country’s health sector has been rocked with a number of problems ranging from drug shortages to theft of medical equipment and drugs by medical personnel. In this interview, our reporter BONIFACE PHIRI speaks to executive director of Health Rights Initiative (HRI), CHARLES NYIRENDA, who proposes a number of ideas on how the sector can be improved.
Q
You recently told the media that theft of drugs and medical equipment by medical personnel in our hospitals started a long time ago. Would you explain your argument?
A
For a long while, a select few have been involved in this repugnant practice. I recall that as I joined the civil service in 1978, I found low level pilferage of drugs and medical equipment in the hospital I worked at. However, for those that got caught during the single party era, the punishment meted out was quite severe; it included prison terms of between five and 14 years, depending on the value of the stolen items. The onset of the multi-party period brought with it an opening up of floodgates, so to speak; the penalties disappeared and the problem graduated from bad to worse. That is generally where we are at the moment.
The problem of drug shortages commenced in 1995 on grounds that a Revolving Drug Fund of 400 000 British pounds set up in 1968 meant for the Medical Stores to buy drugs for hospitals was becoming insufficient to enable Medical Stores to procure enough supplies for all hospitals. By and by, with rising inflation and a steep plunge of the kwacha, things got very bad. When the situation looked hopeless, a series of consultations among stakeholders i.e. Ministry of Health, hospitals, donors and Medical Stores produced a solution. This involved the recapitalisation of Medical Stores by donors and an increase in funding for the drug budget for each hospital on condition that subsidies would go and hospitals would start paying for the commercial value of the drugs plus 15 percent mark up as administration fees. This brought about a significant improvement in the situation of drug supplies. Since then, the main challenge has been inadequate funding to Medical Stores to buy enough drugs even when hospitals have money to procure supplies.
QOne of your proposals is that government should put in place a mechanism where people should be paying for services in public hospitals. Is this not going to be prohibitive for the poor man?
A
What I am insisting on is that the current state of affairs has become untenable and we cannot continue pretending that all is well when the opposite is true. At the moment, there is no question that the health needs of Malawians are not being served well. Ever rising drug costs are exacerbated by the plunging value of the kwacha which means that the situation of drug shortage (against a backdrop of insufficient funding) has come to stay. As I have argued elsewhere, the absence of identity cards is making matters worse because Malawi is treating millions of foreigners from border districts over and above the 14 million-plus locals. That’s why I am advocating a form of cost-sharing scheme that is designed to filter out abuse but at the same time protect the poor.
Q
Do you have examples of countries where the cost-sharing scheme has worked?
A
In countries such as Kenya, they successfully operated such a scheme that provided for a fee exemption for chronic conditions and waivers for those who at a given time couldn’t afford to pay. Once their economic situation changed positively, they then had to start to pay fees. After all, we already practise positive discrimination for the vulnerable households over fertiliser subsidy that only targets those who are worse off. By the same token, it is not correct to assume that all people are too poor to pay a fee for health services. By the way, in 1995 I was one of the delegates who visited Kenya to see how the cost- sharing system was operating and sensitisations of hospital staff took place in a number of seminars here at home. Soon afterwards, government developed cold feet and talk of introducing the scheme evaporated into thin air. On the ground though, there has been no plausible solution to the problem and things have got terribly bad with no light at the end of the tunnel.
Q
How does age distribution, population and cross border out flows affect the health sector’s performance?
A
Age distribution affects the health budget in different ways. The young and the old are generally more expensive to treat and the higher the population the more demands and pressure exerted on the system. That in turn requires extra resources for quality delivery of health services. With our open borders, the situation is aggravated because the health budget does not cater for them. Consequently, the Ministry of Health is unable to offer quality care to the sick.
Q
Your proposal that government should introduce a universal medical insurance has attracted mixed reactions. How significant could this be to our country in terms of improving health standards of people in the country?
A
Universal Medical Insurance would bring in much needed resources to the ever tight health budget. Right now, those opposed to such an initiative are not offering any workable measures to improve matters. All over the world costs of medical services are increasing and for the quality of services to be maintained, infusion of resources is an imperative. Without doing so, there can be no improvement in the situation. From my experience and close liaison with serving public sector health managers, I would estimate that the health sector is receiving below 40 percent of what is required for delivery of quality services. Each year, we find that in real terms, the health budget continues to dwindle. It is for this reason that I propose alternative means of boosting the resources for the health sector apart from government budget funding which can never be adequate. The issue has turned into a medical emergency and it warrants immediate public debate. I know government would be reluctant to provoke the wrath of the people by mentioning introduction of fees in our hospitals, but I don’t think that it has much of an alternative apart from getting brave like it did when it devalued the kwacha in 2012. The immediate impact will be negative, but ultimately there should be an improvement in the delivery of health services.