‘Baylor’s anti-HIV/Aids work offering children hope’
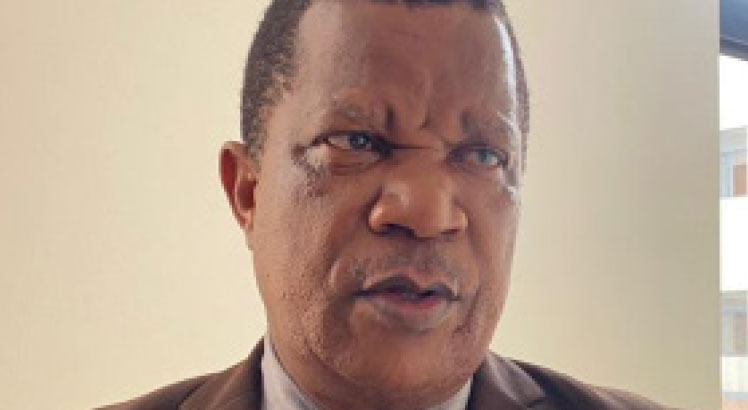
Since it was established 11 years ago, Baylor College of Medicine -Children’s Foundation Malawi (BCM –CFM) in Lilongwe has proved to be a lifeline for children born HIV-positive. The college is largely the reason why there has been a great improvement in the care, advocacy and the survival of HIV-infected children. Our Bureau Chief, SAMUEL CHUNGA, caught up Baylor College executive director, Dr. Peter Kazembe, to find out how Malawi has moved from a time when children were excluded by government policy from accessing life-prolonging ARV treatment to now, where the expectation is that any facility that provides adult ARV services should also be providing ARVs to children. Excerpts:
Your institution in Lilongwe has treated and nurtured many children who were born HIV-positive. Just how many such children are you taking care of and where does Malawi stand, compared with other countries?
HIV continues to be a major global public health issue. It is estimated that 36.7 million people are living with HIV [including 1.8 million children], with a global HIV prevalence of 0.8 percent. Malawi accounts for four percent [980 000] of the total number of people living with HIV in Sub-Saharan Africa. BCM-CFM has now been operating in Malawi for about 11 years with a population of 9 384 ever-registered patients. The current active cohort is 3 616 of which 3 126 [86.4 percent] are on ART. Of the total number of patients on ART at the college’s Abbott Fund Children’s Clinical Centre of Excellence [COE], 2 110 are children. Currently, the country’s ART coverage for children stands at 65 percent, with the BCM-CFM servicing 4.0 percent of this population. Viral load suppression rates for the adolescents in the country stands at 68 percent, while that of the COE stands at 81 percent.
In these days when pregnant HIV-positive mothers access drugs that prevent children being born with the disease, what does it mean for some children still being born HIV-positive?
All babies born to mothers with HIV are classified as “exposed babies” and, as such, are, immediately after birth, supposed to be started on nevirapine, an anti-retroviral (ARV) drug until at six weeks when they are tested to see if they are infected. This is not the standard rapid HIV test but it is a special test called DNA PCR, results of which come back after about a month. If positive, the baby is started immediately on ART as well as on bactrim. However, if the baby’s result is negative and the mother is still breast-feeding, then the baby continues on bactrim only, until the age of one year, when the baby is tested again, this time using the normal rapid test. Where the mother is taking ARVs, both in pregnancy and during breast feeding (known as option B plus), the chance of transmission of HIV to the baby is very small –but is still there.
When and how are children born HIV-positive most vulnerable?
With early initiation of ARV treatment, children can lead normal lives, so long as adherence to medication is good. The current newly-adopted policy is that of “test and treat” or “test and start.” It means that if the HIV test is positive, treatment should be initiated immediately, irrespective of the status of the patient’s immunity. Thus, the CD4 count will ensure that children are started on treatment before the harmful effects of the HIV infection manifest themselves in terms of stunted growth and possible other developmental delays.
The teenage/ adolescent years are the most risky period for our patients’ lives because of multiple factors, including peer pressure, finding time to take their daily medication, especially if they have to go to boarding school, without being asked why they are taking daily medication. Coping with a chronic illness during the adolescent period is difficult enough. But then when they have to deal with a disease that also has stigma attached to it, this adds another layer of difficulty for the adolescents.
What challenges do the pupils and students face, including stigma, and how do you assist the children?
Mostly, these pupils and students experience psychosocial issues that are related to HIV due to a number of factors. These include inadequate support from teachers and fellow students. Most teachers have inadequate knowledge, skills and techniques to support these students. Storage of drugs and privacy when a student wants to take medication is also a challenge, especially in boarding schools. Usually, these challenges result in poor adherence, depression, fear, poor performance, dropouts, relationship problems and other challenging behaviours. The school life skills syllabus is also not HIV-friendly to these pupils and students because it does not take into consideration the therapeutic approach for those learners living with HIV. As such, it becomes a source of self-stigma and discrimination. There are also cases of accidental disclosure due to increased publicity of ART drugs.
Baylor College of Medicine, as an institution, does provide both individual and group counselling sessions to these teens. We also continue conducting ‘HIV and Aids Skills Building training sessions to teachers and prefects in different schools.