Demystifying mental health issues
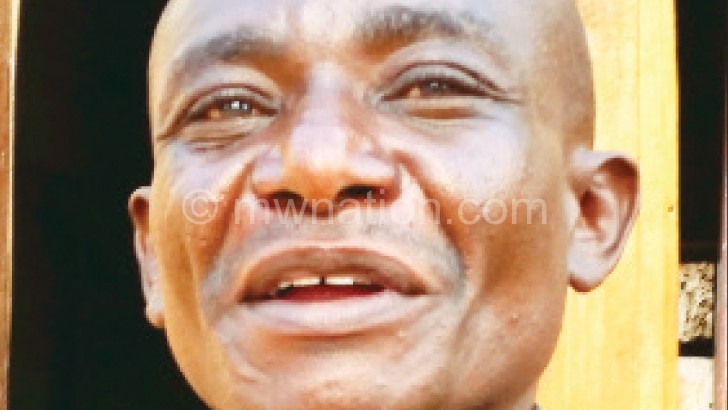
When the stress and anxiety from the pain of losing his parents and later testing HIV positive took its toll on Ted Munthali, 37, from Traditional Authority (T/A) Jalavikuba in Mzimba, his behaviour took a turn for the worse.
He left home, wandering about the peripherals of Mzuzu City where he was eating from garbage bins. That was the beginning of his madness.
“It started like a dream. I used to hear voices calling for my life and I felt the need to run for my dear life and hide from my invisible pursuers,” Munthali recalls.
Now a member of Mzuzu’s St. John of God Mental Health Users Association, Munthali insists he had never smoked before he went into a state of mental breakdown. He attributes to the lapse to the stress he encountered at the loss of his parents that rendered him and his four siblings hopeless orphans.
Today, Munthali is in his right state of mind and employed as a security guard at Lunyangwa Research Station in Mzuzu. He says there is life after mental illness.
“The most important thing is to seek treatment. Those that once experienced mental health problems can still be productive after getting treatment,” he says.

College of Medicine clinical psychologist Chiwoza Bandawe says some pointers that could help identify mental health problems are depression and anxiety.
“There are always notable changes such as memory loss, lack of concentration, tiredness and withdrawal, among many others. It is always important to find out if there have been any pressures which someone has not been able to cope with when such signs are noted,” observes Bandawe.
Statistics from the Ministry of Health (MoH) indicate that Zomba Mental Hospital, Bwaila Psychiatric Unit and St John of God Community Services of Mzuzu admit approximately 2 000 patients a year. The three centres attend to over 20 000 clients as outpatients in a year.
Clinical psychologist at St John of God in Mzuzu, Devlin Silungwe, says mental health problems are common and they include stress, which is common in relationships and jobs.
“These are commonly associated with social problems. For example, when you cannot focus at work because you are too broke to feed your family, those are mental health problems,” he says.
Silungwe says such problems require treatment but mostly they call for counselling and psychotherapy.
He says commonest health illnesses are put in different categories.
“Mostly the one that is commonly called madness or psychosis in scientific terms, is the smallest in terms of percentage of all mental health problems,” he says.
Silungwe says in psychosis, patients are completely disturbed in their thinking or have a split mind where they fail to rationalise and differentiate right from wrong.
Munthali is grateful for the treatment he received at St John of God.
“People thought I had smoked hemp but it was not that. Since 2004, I have been taking my treatment and life has been normal,” says Munthali.
MoH spokesperson Adrian Chikumbe calls for mindset change if people with mental health problems are to get properly assisted.
“When one develops signs of mental illness, the person has to be taken to a health facility for assessment,” he explains.
Chikumbe says it is the health facility that will determine the next course of action depending on their findings, which might include referral to the next level of care.
But in a country where some mentally ill people roam the streets, sometimes committing crimes and causing harm to innocent people, health authorities believe the situation needs a collaborative approach.
“As a ministry, we encourage care givers or guardians to bring their relatives to hospitals. In this way, there is continuity of care after discharge from the hospital,” explains Chikumbe.
He says the MoH’s focus is to integrate mental health services into primary and secondary health care services with the aim of managing patients close to or within their community for continuity of the care but also to reduce related stigma.
Silungwe emphasises the need for community involvement in dealing with mental health issues.
“Mental illness is a human rights issue, we expect people to take their sick relatives to hospital and not expect hospitals to hunt down patients. Anywhere it doesn’t work like that.
“Hospitals do not go out hunting for malaria patients for example. There are legal issues involved, What if you take in someone who tells you he was conducting a research?” queries Silungwe.





