Long walk to access ARVs
Ease of access to health care is of great importance in any country but particularly for villagers living with HIV and Aids. However, some HIV patients in Blantyre are being forced to walk long distances of up 20 kilometres to collect their quarterly allocations of anti-retroviral (ARV) drugs as BOBBY KABANGO found out:
The death of a mother of three from Babanango, South Africa in 2017 speaks volumes about how unforeseen travel costs to and from hospitals can be an obstacle to getting ARV medication. She was travelling a distance of about 18 kilometers to get the lifesaving drugs.

Her predicament is also faced by many patients living in rural areas in Malawi.
On February 6 this year at around 10 o’clock in the morning I met Cecelia Chigalimoto from Chikhombo village in Group Village Headman Nzeru, Traditinal Authority (TA) Somba, Blantyre district walking to the hospital.
She is 49-years-old, rugged and weak. But she pushed on.
There is no health facility in Nzeru’s area, the nearest one is some 20 kilometres (km) away.
“I have to walk to the hospital. There is no other means,” she says as she made her way in the sweltering heat to Pensulo Clinic.
The situation in the area becomes worse during the rainy season as the roads to the clinic where they collect the drugs become muddy and flooded. This means one has to find an even longer but navigable route on foot.
“Most of the time there is no vehicle that reaches the clinic from our village,” she explains. “When going to our village, one has to board a minibus going to Sigerege and from there you proceed on a hired motor bicycle.
This means the only solution for Chigalimoto is to hire a motorbike to drop her at the health centre at a cost of K5 000 return trip.
“I am too poor to raise such money, so I gather my strength and walk,” she says as she takes a rest under a shade.
She unwraps her Chitenje and unknots the corner of the cloth to show me a worn out K50 bank note.
“The only money I have on me today is K50,” she says. “This is the only money I have. Someone gave me the money yesterday, so that I can buy a snack since I have stayed two days without food.”
Chigalimoto leaves home around 5 am in the morning to go to Pensulo Clinic. She arrives at the health centre around 11am.
Another woman is Margret Mabvuto from Chikhombo Village. She was diagnosed with HIV in 2014.
Just like Chigalimoto, Mabvuto always walks about 20 km to access the lifesaving drugs.
Mabvuto, 55, is too poor to raise money for a motorcycle going to the hospital.
“Every time I take ARVs, I take four tablets every day. Meaning I need to have them every time. So we face challenges to access the treatment,” she said. Her village has about 30 people who are on treatment.
But Group Village Mpagaja is not happy with the situation facing her people. She explains that villagers surrounding Chiringani area in Blantyre need a health facility so that they can easily access health services including ARVs.
“My subjects are forced to travel to Chilomoni Health Centre… it’s about 20 kms all else another way is to go to Pensulo clinic in T/A Kumtaja,” she says.
The chief explains that they have been petitioning government and their Member of Parliament (MP) to consider erecting a health centre in the area but nothing has happened so far.
“The only things we access so quickly are election materials, but after voting, we do not access other basic needs,” she says angrily.
The difficulties associated with one collecting their ARVs have made many people to default on their medication.
The country’s Ministry of Health (MoH) recommends that patients should not walk more than 5 km to access a health facility. This distance has been revised from eight kilometers.
The Malawi Health Equity Network (Mhen) executive director George Jobe is worried that subjecting people to such long distances might frustrate the gains Malawi has made in dealing with the HIV and Aids pandemic.
“Currently, there is need to intensify outreach clinics that health workers travel and serve the people right there in the remote or hard-to-reach areas. The health workers should either use vehicles, motor cycles,” says Jobe.
He says the Malawi annual health budget should be responding to the country’s commitments, legislation and policies.
“The budgets should always include construction of health facilities in some more hard-to-reach areas where people walk long distances to access health facilities. Because walking long distances to a health facility puts Malawi and Malawians at risk.
“As a nation we may experience people who default treatment thereby retrogressing to old poor indicators in HIV and Aids status. In addition, such distances are an economic hardship to people because they sometimes need money for transport to travel, or it is another health hazard as they overwork to walk such distances,” he explains.
Jobe thinks Malawi has made tremendous and commendable gains in the fight against HIV and Aids, “and as a country we cannot afford to go back to the 1990s when many people died due to lack of affordable health care and HIV drugs.”
According to a 2017 Global Information and Education on HIV and Aids, Malawi has one of the highest HIV prevalence’s in the world despite the impressive progress the country has made in controlling the scourge in recent years.
The report says young people are particularly at risk, due to early sexual activity and marriage, with 50 percent of new HIV infections affecting those aged 15 to 17 in Malawi.
The country has over one million people living with HIV, the report shows, and among them, 9.6 percent are adults (15-49) and 39 000 new HIV infections.
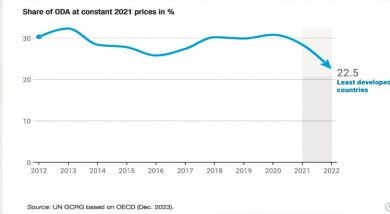
The report further shows that Malawi is one of the least developed countries receiving more funding to fight the disease.
In 2016, Malawi received 74 per cent of funding for its HIV response from the Global Fund to Fight Aids, Tuberculosis and Malaria and the Presidents Emergency Plan for AIDS Relief (Pepfar) and a further 12 percent from other donors, with the remaining 14 per cent coming from domestic funding.
“Significant progress has been made on the proportion of domestic funds being made available for the HIV response,” reads the report in part.
Yet despite all the funding patients in Chiringani area struggle to benefit from free ARVs drugs as they walk for 7 hours to access the drugs.
“Government needs to intervene, we need a health facility in Chiringani,” pleads Chigalimoto.n